“Her illness won’t go away. She will have it for life.”
He said those words at her appointment last Friday, just as he said them to me at her appointment before that in January. Now matter how many times he says them, they always sting.
“He” is Lukah’s autonomic neurologist, Dr. B, in Chicago. He said those words when Corey made a casual statement about getting rid of her POTS. It’s not what I like to hear from Dr. B, but I appreciate him not sugar-coating it and I so appreciate his expert opinion, as I truly believe he is an expert. There are not many “experts” on autonomic disorders, and I am very grateful to have him as Lukah’s primary POTS doctor only 3 hours away.
There are so few experts, in fact, that most DOCTORS she has seen or I have talked to, have never even heard of POTS. When she has been hospitalized, we have to educate them! Here is a funny video that pretty much sums up the life of a Potsy when seeking medical care:
http://www.youtube.com/watch?v=lg7YvKousDM&feature=youtu.be
Back to Dr. B. . .
Ever so slowly, I’m accepting this opinion of Dr. B’s — even though I do not like it. I know I am accepting it because my goal has drastically changed from this time last year. It has gone from looking for a CURE for what was going on, to instead, looking for ways to make her more comfortable. To me, that is a sign showing I have accepted that The Beast will remain.
I just want her belly aches and vomiting to stop. I want the blinding headaches to stay away. The ones that I can tell she has without asking her just by looking in her eyes. I want her to be able to sleep, instead of suffering from insomnia until 5:30 a.m. I want the urinary tract infections to end. And most of all, I want her passing out/seizure episodes to halt.
What started as seizures and passing out, has turned into so much more than that. It seems each day we are uncovering a new facet of this dreadful disease. Another symptom to chalk up to The Beast. Yet, the seizures and passing out is what I most want to end for her.
And we’re working on just that, with the help of Dr. B.
We had our second visit with Dr. B last Friday. He wanted Lukah to come up so he could do some autonomic testing on her. Even though she has had this testing before, he wanted to retest so he could watch for himself what her body’s reaction to the testing was. . . instead of relying on past medical records to tell her story.
Prior to the testing, he spent a great deal of time with Lukah, talking about how she had been feeling. In addition to talking at length about her seizures and fainting spells, she advised him again of her headaches (almost daily) and stomach aches. She also mentioned strange leg pain that has been happening. It happens on the back of her thighs and also the back of her knees. It is very painful, but it isn’t like muscular pain from working out too hard, and it isn’t when she stands up — only when sitting or laying. He calls it neuropathy, and is yet another complication from POTS.
After spending about 45 minutes with him, we went into the testing room. The testing technician placed electrodes on Lukah’s back and she was hooked up to a high-tech blood pressure and heart rate machine that would constantly monitor both fo these. The first test was a deep breathing test. She had to inhale for 5 seconds and exhale for 5 seconds, and she repeated this 6 times. She got dizzy. No surprise there!
The next test she did is called the Valsalva maneuver. While still hooked up to the machines above, she had to, this time, exhale into a small syringe that looked kind of like a straw. She had to keep the air pressure at 40mm for 15 seconds (which is a long time to breathe out into a straw at a high pressure!). She had to then rest for three minutes and do this 2 more times with a 3 minute rest in-between. She was dizzy each time. Shocking, I know! 🙂
Dr. B came in at this point and the testing technician pointed out a few things on those tests and he nodded and said, “Yes, very signficant.”
It was then time for her tilt table test to start. The tilt-table test is an informative test that can help identify the causes of fainting. The tilt table test places a patient on a table with a foot-support, and then the table upward. The tilt-table may start off in a horizontal position and be tilted by degrees to a completely vertical position. Lukah’s was tilted at about a 70 degree angle. The patient’s blood pressure, pulse, and symptoms are monitored throughout the test.
Here she is all strapped in and ready to be tilted.
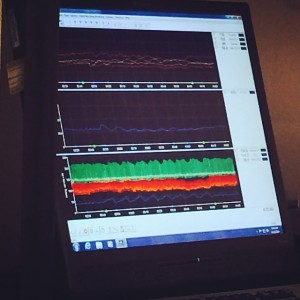
Dr. B stayed in the whole time, watching her body’s reaction. I would watch him shake his head, ask her if she was doing ok, ask her if she was dizzy, then look at the blood pressure readings and shake his head again. Here is what he was looking at when he would shake his head. How smart is he to be able to make sense out of this screen???
Lukah did not pass out this time (she did on one of her prior tilt table tests) but had markedly positive results indicating orthostatic intolerance and increase of heart rate indicative of POTS.
So tell me something new, right? 🙂
Dr. B told us she has the blood pressure of a 65-year-old. To that, Lukah exclaimed, “But I’m only 15!!”
Through this round of testing, Dr. B was able to identify what types of medication he feels will best help Lukah based on how her body reacted to the testing.
In my last post, I talked about how many medications she was on. Dr. B has now opted to change-up her medications, which will reduce the amount she has to take by 2. She will now be on a drug that is actually usually prescribed for ADHD called Tenex. It can help with POTS as it is known to constrict blood vessels.
He also has prescribed a drug that is not available in the USA called Ivabradine. For some reason, it is available in just about every country besides the United States. Lukah’s heart rate is always high (yesterday, while just sitting on the couch, her resting heart rate was 118). The ivabradine actually reduces the heart rate instead of working like other heart medications to reduce or increase the blood pressure. I will be working with a pharmacy in Canada to obtain this drug.
She also was given another heart drug called midodrine. For many “potsies,” this is a miracle drug. I’m hoping for the best.
So, with Dr. B’s help, we are tackling her first symptom — and her most debilitating one . . . her seizures and passing out episodes. But we have many more to conquer. Dr. B knows that, and mentioned bringing other doctors in to the mix (a urologist for example, to help with the frequent urinary tract infections).
While we may bring others into the mix, Dr. B will remain her “chief” as I respect him completely and am so grateful he has shown such kind and caring interest in her case. With him, we will figure this out.
While it may never “go away,” at least with Dr. B’s help, perhaps someday will keep The Beast at bay. And we’ll always keep Looking for Lukah.